
Tracking your hormones can feel like a lot when you are trying to conceive. The luteal phase, also called the secretory phase, is the part of your menstrual cycle that starts after ovulation and ends when your next period begins. It is the window when progesterone rises and prepares the uterine lining for a possible pregnancy. Knowing how long this phase is helps you time intercourse, understand implantation timing, and choose when to take a pregnancy test. You do not need complex tools to work it out. With a few dates and simple maths, you can estimate your luteal phase length and make sense of your cycle patterns. This guide explains what the luteal phase is, how to calculate it, how doctors in Australia assess short or long phases, and practical ways to look after your reproductive health while trying to conceive.
Quick Answers About the Luteal Phase
What is the luteal phase?
It is the time from ovulation to the day before your next period. After the egg is released, the follicle becomes the corpus luteum, which makes progesterone to prepare the uterine lining for implantation.
How long should the luteal phase be?
Most people have a luteal phase that lasts about 11 to 17 days. Less than 10 days can make conception less likely. If pregnancy occurs, the luteal phase continues rather than ending in a period.
How do I calculate my luteal phase?
Note your ovulation date, then count the days until your next period begins. Period start date minus ovulation date equals your luteal phase length. For example, ovulate on day 14 and period on day 28 gives a 14 day luteal phase.
What is the luteal phase in your cycle
A menstrual cycle is often described in two parts, the follicular phase before ovulation and the luteal phase after ovulation. The luteal phase starts when the egg is released and the follicle transforms into the corpus luteum. This temporary gland releases progesterone. Progesterone thickens and stabilises the lining of the uterus, creating a supportive environment for a fertilised egg. This is why the luteal phase is also known as the secretory phase.
Progesterone rises in the days after ovulation. Body temperature commonly increases by about 0.2 to 0.5 degrees Celsius at this time. If pregnancy does not occur, the corpus luteum stops producing progesterone, the lining sheds, and menstruation begins. If pregnancy occurs, early human chorionic gonadotropin from the forming placenta keeps the corpus luteum active until the placenta takes over hormone production.

What happens during the luteal phase?
What affects luteal phase length and hormones
Luteal phase length varies a little from person to person, but it is usually steady within the same person. A phase shorter than 10 days can reduce the time available for implantation. This can happen if progesterone levels are low or if the corpus luteum does not last long enough. Factors linked with a short luteal phase include very low body weight, very high training loads, high stress, thyroid disease, high prolactin, and early perimenopause. Endometriosis and some uterine conditions can also affect implantation conditions, even if luteal length is normal.
Some people worry about luteal phase deficiency, a term sometimes used to describe low progesterone in the second half of the cycle. Research findings are mixed on whether it is a distinct diagnosis. In practice, doctors focus on whether you are ovulating regularly, whether the luteal phase is very short, and whether there are other conditions that may affect fertility. Polycystic ovary syndrome can cause long cycles, but the luteal phase length after ovulation is usually within the normal range. Knowing your own rhythm helps guide next steps.
Calculating your luteal phase length at home
To calculate luteal length, you need two dates. Track your ovulation day, then note the first day of your next period. Subtract the ovulation date from the period start date. If you ovulate on day 15 and your period starts on day 29, your luteal phase is 14 days. This method works best when you can identify ovulation with reasonable confidence.
You can estimate ovulation by watching for fertile cervical mucus, which becomes clear and stretchy as ovulation approaches. Many people use ovulation predictor kits, which detect the rise in luteinising hormone in urine about 24 to 36 hours before ovulation. Basal body temperature tracking is another tool. Use a digital basal thermometer and take your temperature on waking after several hours of sleep. Chart the readings at the same time each morning. A sustained rise after mid cycle suggests ovulation has occurred and marks the start of your luteal phase. Alcohol, illness, and disrupted sleep can change readings, so keep notes to interpret your chart.
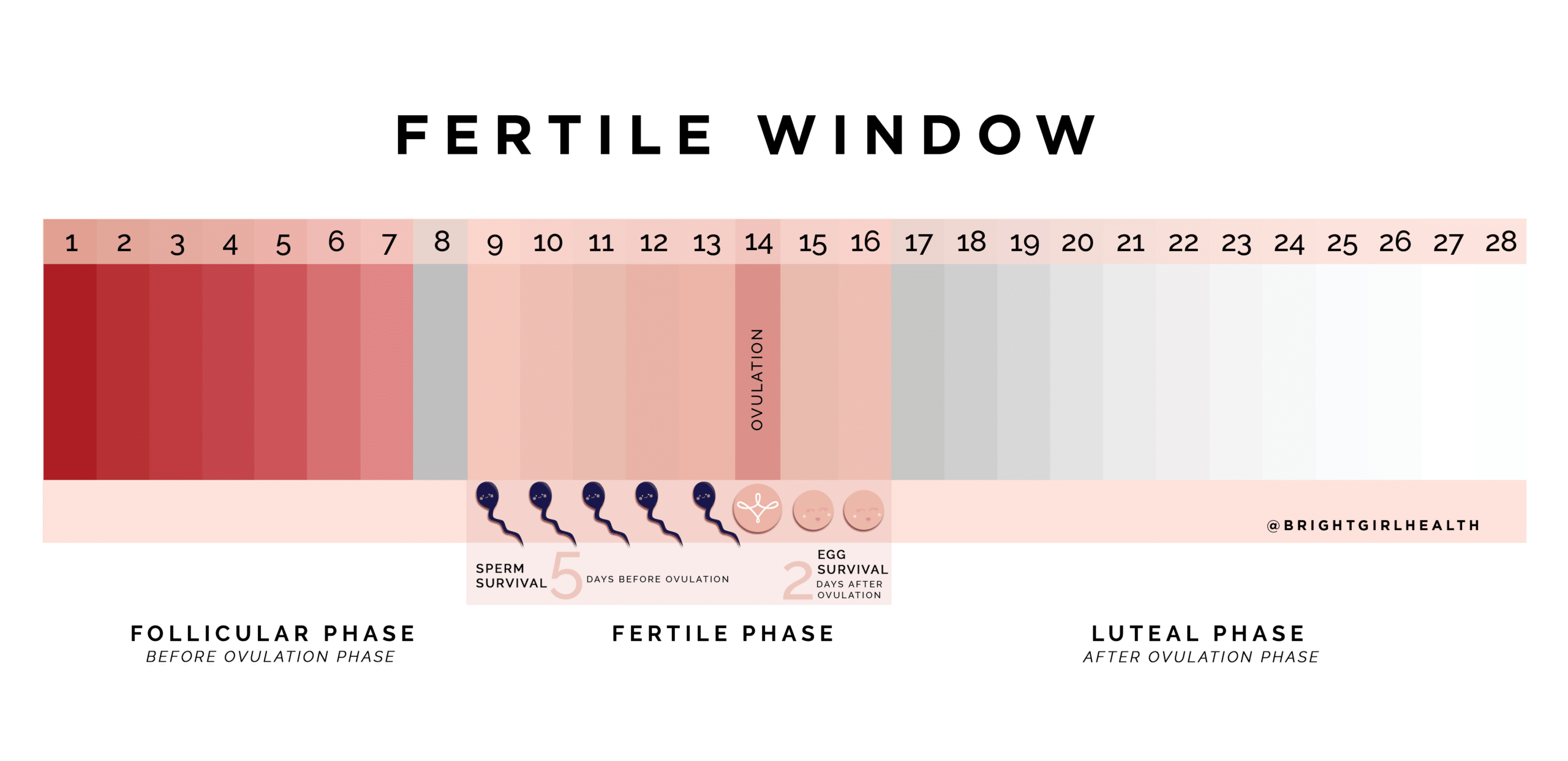
Image courtesy of The Bright Girl Guide by Demi Spaccavento .
Diagnosis and testing in Australia
If your cycles are regular and your luteal phase is between 11 and 17 days, that usually fits within the expected range. If your luteal phase is consistently shorter than 10 days, if you are not sure you are ovulating, or if you have other symptoms such as heavy bleeding or severe pelvic pain, book a review with your GP. Your GP will ask about cycle history, medical conditions, medications, and lifestyle. They may arrange blood tests and imaging, and discuss referral pathways if you have been trying to conceive without success.
Common tests include a mid luteal progesterone blood test, thyroid function tests, and prolactin. The mid luteal test is timed to around seven days after ovulation rather than a fixed cycle day. For example, if you ovulate on day 17, the test is usually done on day 24. An ultrasound may be requested to assess the ovaries and uterus. If you have been trying for a baby for some time, your GP may also discuss a semen analysis for your partner. In Australia, GPs often coordinate initial testing, and refer to a fertility specialist if needed.
What the tests involve and how results are used
A progesterone blood test takes a small sample from a vein in your arm. Results are interpreted in the context of your cycle timing. A mid luteal progesterone level consistent with ovulation supports that the corpus luteum is active. If the level is low at the wrong time, your GP may repeat the test with better timing. Thyroid and prolactin tests help detect conditions that can disturb ovulation or luteal function. A pelvic ultrasound may be transabdominal, transvaginal, or both, and is used to view the endometrium and ovaries. The sonographer will talk you through the steps and a report is sent to your doctor.
Results guide next steps. If you are ovulating and the luteal phase is in range, reassurance and timed intercourse may be all that is needed. If there is a short luteal phase or another condition is found, treatment is tailored to the cause. Your GP or specialist will explain benefits and possible side effects before any treatment is started.
Managing a short luteal phase at home
Healthy routines support hormone balance. Aim for regular meals with protein, vegetables, whole grains, and sources of healthy fats such as avocado, olive oil, and nuts. Include foods rich in omega 3 like flaxseed and oily fish. Keep caffeine and alcohol moderate. Do not smoke or vape if you are trying to conceive. A steady sleep routine of about seven to nine hours supports normal hormone rhythms. Regular movement such as brisk walking, swimming, yoga, or pilates can help. If you train at a very high level and have short cycles or missed periods, discuss a plan with your GP.
Some people consider supplements. A daily prenatal vitamin can cover key nutrients while you are trying for a baby. Speak with your doctor or pharmacist to choose a product that suits your needs. If your GP diagnoses low progesterone, they may consider prescription progesterone in oral, vaginal, or injectable forms. Side effects can include headache, bloating, breast tenderness, nausea, or tiredness. hCG injections are sometimes used in specialist care to support the corpus luteum, though this is not needed for most people. Always discuss risks and benefits with a qualified clinician.

Conceive Plus Women’s Fertility Support is the best prenatal vitamin in Australia to assist conception.
When to see a GP or fertility specialist in Australia
If you are under 35 and have tried for a baby for 12 months without success, see your GP for an assessment. If you are 35 or older, see your GP after 6 months of trying. Seek earlier review if your cycles are very irregular, if your periods are very heavy or very painful, if you have had pelvic infections or surgery, or if you have had two or more early miscarriages. See your GP promptly if you have signs of thyroid disease such as unexplained weight change, heat or cold intolerance, or marked fatigue.
In Australia, your GP can arrange initial tests and refer you to a gynaecologist or fertility specialist for further care. Some public hospitals offer fertility clinics for eligible patients and there are private clinics across the country. Ask about costs, waiting times, and what tests are recommended before treatment. If you need support with cycle tracking, many practices have nurses who can help you set up a plan.
How ovulation and pregnancy tests fit into tracking
Ovulation predictor kits detect the surge in luteinising hormone in urine, which usually precedes ovulation by about one to two days. A positive result tells you that ovulation is expected soon. Time intercourse on the day of the surge and the following day to cover the fertile window. Record the surge date and then count the days until your next period to calculate your luteal phase. This gives a practical luteal phase calculator using your own data.
Basal body temperature can confirm that ovulation has already occurred. A sustained temperature shift helps mark the start of the luteal phase on your chart. A mid luteal blood progesterone test provides clinical confirmation in cases where it is needed. Home pregnancy tests detect hCG in urine after implantation, which typically happens about 6 to 10 days after ovulation. Testing is more reliable from the day your period is due. If you prefer home tracking tools, Fertility2Family offers fertility kits that include ovulation and pregnancy tests so you can align testing with your cycle data.
Frequently Asked Questions About the Luteal Phase Australia
Is the luteal phase always the same length each cycle
It is usually steady for an individual, with small variation of a day or two. Large swings from month to month suggest irregular ovulation or another factor worth checking with your GP.
Does spotting in the luteal phase mean I cannot get pregnant
Light mid to late luteal spotting can happen and does not always mean a problem. Frequent spotting or spotting with pain should be discussed with your GP to check for conditions such as polyps or endometriosis.
Can I lengthen a short luteal phase naturally
Healthy weight, regular sleep, manageable stress, and balanced nutrition support normal ovulation and luteal function. If the phase remains short, see your GP as medical causes such as thyroid or prolactin issues may need treatment.
Does breastfeeding change the luteal phase
During breastfeeding, prolactin can suppress ovulation or shorten the luteal phase. Cycles often normalise as feeding reduces. If you wish to conceive while breastfeeding, talk with your GP about realistic timelines.
How does PCOS affect the luteal phase
PCOS can cause infrequent ovulation and long cycles. Once ovulation occurs, the luteal phase length is often within the typical range. Cycle tracking can help identify ovulation so timing is clearer.
When should I do a pregnancy test if I have a long luteal phase
If your period is late, test from the day your period is due or later. A positive appears after implantation and hCG rise. If tests remain negative and your period does not arrive, see your GP.
Fertility support for your next steps
Your cycle is personal, yet patterns become clear once you record them for a few months. If you track ovulation with urine LH tests and basal body temperature, and note your period start date, you can calculate your luteal phase and plan the right days for intercourse. This reduces guesswork and helps you decide when to take a pregnancy test. If your phase is short or your cycles are irregular, reach out to your GP. Early checks for thyroid function, prolactin, and ovulation markers can save time and guide simple steps that make a real difference.
Fertility2Family is here with practical tools and plain language advice. Our blog explains cycle phases, hormone changes, and home tracking. If you want ready to use supplies, our fertility kits bundle ovulation and pregnancy tests so you can track with confidence. For medical questions, partner with an Australian GP or fertility specialist who can tailor care to your health and goals.
References
https://www.healthdirect.gov.au/menstrual-cycle
https://www.healthdirect.gov.au/ovulation
https://www.healthdirect.gov.au/pregnancy-tests
https://www.jeanhailes.org.au/health-a-z/periods/menstrual-cycle
https://www.jeanhailes.org.au/health-a-z/fertility/trying-to-conceive
https://www.betterhealth.vic.gov.au/health/healthyliving/menstruation-and-the-menstrual-cycle
https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/infertility-female-causes-of
https://www.qld.gov.au/health/staying-healthy/sexual-health/pregnancy/trying-for-a-baby
https://ranzcog.edu.au/womens-health
https://www.racgp.org.au/afp/2012/december/infertility-in-practice


