Do You Ovulate on the Pill? Facts & Insights Explained
Birth control pills are among the most researched contraceptives worldwide and remain a common choice across Australia. Many people want to know whether ovulation still happens on the pill, why withdrawal bleeding looks different to a period, and how missed tablets or other medicines might change protection. In short, combined oral contraceptive pills usually stop ovulation by keeping oestrogen and progestogen at steady levels. Progestogen only pills mainly thicken cervical mucus and may also stop ovulation if taken at the same time every day. Bleeding during the break is a response to a drop in hormones rather than a natural period. This guide explains how the pills work, when ovulation can slip through, how to handle missed doses, and when to see a GP or sexual health clinic in Australia. You will also see where home tests fit, including ovulation tests and pregnancy tests if you are coming off the pill or worried about a late bleed.
Quick Answers About Ovulation on the Pill
Do you ovulate on the pill? With correct daily use, combined pills suppress the luteinising hormone surge that releases an egg, so ovulation usually does not occur. Progestogen only pills may also block ovulation but are more time sensitive.
Is withdrawal bleeding a period? No. Bleeding in the tablet-free days is triggered by a drop in synthetic hormones. It is not the same as a natural period that follows ovulation.
Can you get pregnant on the pill? Yes, but the risk is low with perfect use. Missed or late pills, vomiting, diarrhoea, and certain medicines can allow ovulation and reduce protection. Use condoms and seek advice if this happens.
What Happens to Ovulation on the Pill
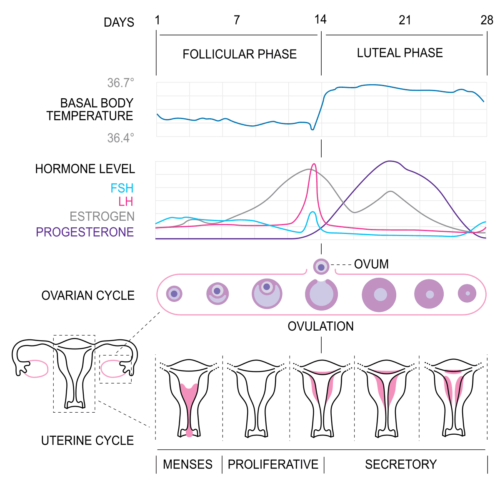
The menstrual cycle depends on signals between the brain and the ovaries. A surge of luteinising hormone prompts the ovary to release a mature egg. Combined oral contraceptives keep oestrogen and progestogen at steady levels, which quiets these signals and prevents the luteinising hormone surge. Without the surge, the ovary does not release an egg.
Progestogen only pills mainly thicken cervical mucus so sperm cannot pass as easily. Some people on progestogen only pills also have ovulation blocked, but this is less consistent and relies on very strict timing. The pills also make the uterine lining thinner so a fertilised egg is less likely to implant.
These effects explain why regular use matters. Small hormone dips from missed tablets can be enough to allow the brain to restart signals, which can lead to breakthrough ovulation in some situations.

How Combined and Progestogen Only Pills Work in Practice
Combined oral contraceptives contain synthetic oestrogen and progestogen. By keeping hormone levels steady, they stop ovulation and also thicken cervical mucus. They remain effective with some timing flexibility. If you are starting a combined pill, use condoms for the first seven days while suppression builds.
Progestogen only pills do not contain oestrogen. They mostly work by thickening cervical mucus and may also block ovulation if taken at the same time every day. Timing is strict. A late dose can allow mucus to thin and hormone levels to dip. When beginning a progestogen only pill, use condoms for the first 48 hours.
Australian guidance supports these time frames and encourages checking a current product leaflet or a pharmacist for brand-specific rules. If you are unsure which pill you take, your GP or sexual health clinic can confirm the type, dose, and the best way to take it for your routine.

When Ovulation Can Still Happen
Breakthrough ovulation is uncommon with correct use but can occur. The most frequent reason is missed or late tablets. Skipping pills or taking them at irregular times can drop hormone levels below the threshold needed to suppress the luteinising hormone surge. Illness with vomiting or severe diarrhoea within a few hours of a dose can have the same effect because the pill may not be absorbed.
Some medicines speed up the breakdown of contraceptive hormones in the liver. Rifampicin for tuberculosis, some older anticonvulsants such as carbamazepine, and the herbal product St John’s wort are well known examples. These can lower hormone levels and increase the chance of ovulation and pregnancy. Always ask a pharmacist or GP about interactions if you start a new medicine or supplement.
Individual metabolism can vary. A small number of people may process hormones faster, which can increase the impact of missed tablets. If you have concerns about symptoms or timing errors, speak to your GP, a pharmacist, or a family planning service for tailored advice.

Withdrawal Bleeding, Periods, and What That Bleed Means
Bleeding during the tablet-free days, or during placebo tablets, is called withdrawal bleeding. It starts because synthetic hormone levels fall when you pause active tablets. This is different from a natural period, where ovulation triggers hormone rises and falls that build and then shed the uterine lining. On the pill, the lining usually stays thin, so withdrawal bleeding is often lighter and shorter.
Some people choose to skip the tablet-free interval by taking active tablets continuously for longer stretches. This is safe for most people after discussion with a GP and often reduces cramps and bleeding. If you notice very heavy bleeding, bleeding after sex, new pain, or bleeding between tablets that lasts, book a check with your GP to rule out other causes.
If you are unsure whether you have had a real period, remember that a true period follows ovulation. When ovulation is suppressed by combined pills, the monthly bleed is a scheduled withdrawal rather than a sign of fertility returning that month.

Testing and Tracking While Using the Pill
Ovulation predictor kits detect the luteinising hormone surge that triggers egg release. Combined pills are designed to stop this surge. That means ovulation kits are not helpful while actively using the pill. If you are coming off the pill and trying for pregnancy, ovulation tests and fertility tracking apps can help time intercourse once your natural cycle resumes.
Pregnancy testing has a clear role if you miss pills or develop symptoms such as new breast tenderness, nausea, or a delayed withdrawal bleed after timing errors. Use a home test if your withdrawal bleed is late or lighter than usual after missed tablets. Repeat a week later if the first test is negative and you still have no bleed.
If you plan a switch to a long acting method, such as an implant or an intrauterine device, your GP or family planning clinic can time the change to maintain protection without gaps.
Missed Pills, Medicines, and What To Do Next
If you miss one combined pill, take it as soon as you remember and take the next one at the usual time. You may take two on the same day. If you miss two or more in a row, take the most recent missed tablet, continue the pack, and use condoms for the next seven days. If unprotected sex occurred in the days before or after the missed tablets, seek advice about emergency contraception.
For the progestogen only pill, take a late or missed tablet as soon as you remember and use condoms for the next 48 hours. If you are more than three hours late, protection can drop. Some newer progestogen only pills have a longer window, so check your brand or ask a pharmacist.
Vomiting or severe diarrhoea within about three hours of taking a tablet can reduce absorption. If this happens, follow missed pill advice and use condoms. Medicines such as rifampicin, some anticonvulsants, and St John’s wort can lower hormone levels. Ask your GP or pharmacist about interactions before you start a new medicine or supplement, and use extra protection if advised.

When To See a GP or Sexual Health Clinic in Australia
Book a review if you have repeated timing issues, new bleeding patterns that worry you, pain with sex, or suspected pregnancy. Seek urgent care for chest pain, sudden shortness of breath, one sided leg swelling or pain, or severe headache with vision changes. These can be signs of a blood clot or migraine with aura and need prompt assessment.
Discuss your pill choice if you smoke, are over 35, have a history of migraine with aura, have high blood pressure, or a family history of clotting disorders. Your GP may suggest a different pill or a non oestrogen method. People with conditions such as polycystic ovary syndrome, endometriosis, or acne can also discuss symptom control with tailored pill choices.
If you stop the pill to try for pregnancy, most people ovulate again within one to three months. If cycles have not returned by six months, see your GP. Family planning services across Australia offer counselling on contraception choices, switching methods, and fertility planning.
Frequently Asked Questions About Ovulation on the Pill Australia
What happens to my eggs while I am on the pill? Your ovaries keep a supply of immature follicles. Combined pills usually pause their growth by blocking the brain signals that start ovulation. The eggs are not used up faster or harmed by the pill.
Can I use the pill for period control without a monthly bleed? Yes. Many people safely run packs back to back to reduce or skip withdrawal bleeding. Speak with your GP about a plan that fits your health and brand.
Do acne and cramps improve on the pill? Many combined pills reduce acne and period pain by stabilising hormones and keeping the uterine lining thin. If side effects occur, your GP can adjust the formulation.
How soon is the pill effective when I start? For a combined pill, use condoms for the first seven days unless you start on day one of bleeding. For a progestogen only pill, use condoms for 48 hours from the first dose.
Are ovulation tests useful while on the pill? No. Combined pills suppress the luteinising hormone surge. Ovulation kits will not give helpful results until your natural cycle returns after stopping the pill.
What if I take antibiotics? Most antibiotics do not affect pill hormones. Rifampicin is an exception and lowers levels. Always check with a pharmacist about interactions and use extra protection if advised.
How Australian Guidance Supports Safe, Effective Use
Across Australia, contraceptive care follows clear standards so people can choose the method that suits their health, lifestyle, and plans. GPs, pharmacists, and family planning services provide advice on starting, changing, and safely skipping withdrawal bleeds. They also help with real life issues such as travel, new medicines, shift work, and heavy periods.
If you need to time conception, consider how home testing fits your stage. While on the pill, ovulation kits are not useful. If you have stopped the pill and want to track your fertile window, ovulation tests can help once cycles return. If you miss pills and worry about pregnancy, a home pregnancy test offers fast reassurance. For ongoing support, local services such as Family Planning NSW, Sexual Health Victoria, and Healthdirect provide reliable guidance and help you find a nearby clinic. If your needs change, your GP can discuss long acting options such as implants and intrauterine devices that remove timing pressure.
References
https://www.healthdirect.gov.au/contraceptive-pill
https://www.healthdirect.gov.au/contraception
https://www.healthdirect.gov.au/what-to-do-if-you-miss-the-pill
https://www.fpnsw.org.au/health-information/contraception/combined-oral-contraceptive-pill
https://shvic.org.au/for-you/contraception/contraceptive-pill
https://www.jeanhailes.org.au/health-a-z/periods/contraception
https://shinesa.org.au/you-and-your-body/contraception
https://www.sahealth.sa.gov.au/wps/wcm/connect/public+content/sa+health+internet/health+topics/health+conditions+prevention+and+treatment/sexual+health/contraception
https://www.true.org.au/Contraception
Evan Kurzyp
Evan is the founder of Fertility2Family and is passionate about fertility education & providing affordable products to help people in their fertility journey. Evan is a qualified Registered Nurse and has expertise in guiding & managing patients through their fertility journeys.