Waiting to see if this cycle leads to pregnancy can be exciting and stressful at the same time. The two-week wait is the time between ovulation and the expected period, and it is when the body prepares for possible implantation. Hormones shift, symptoms can appear or stay quiet, and at-home tests may be tempting. This guide explains what usually happens after ovulation, when pregnancy tests are most reliable, and when to see a GP in Australia. You will find plain-language explanations of hCG, progesterone and early symptoms, plus practical tips for self-care. The aim is to help you feel informed and calm, using guidance aligned with Australian health services so you can decide what to do next with confidence.
Quick Answers About the Two-Week Wait After Ovulation
When should I take a pregnancy test after ovulation?
Most people get the clearest result from 14 days after ovulation or from the first day of a missed period. Testing earlier can give a negative result even if pregnant. Use first morning urine. If negative and your period has not started, wait 48 hours and test again.
What symptoms are normal in the two-week wait?
Sore breasts, mild cramps, bloating, fatigue, mood changes and feeling warmer can occur due to progesterone, with or without pregnancy. Some people feel no symptoms and still conceive. Symptoms alone cannot confirm pregnancy.
Can implantation bleeding happen?
Light spotting can occur between day 6 and day 10 after ovulation when the embryo attaches to the uterus. It is usually lighter and shorter than a period. Many people never notice it. Seek care if bleeding is heavy, painful or linked with dizziness or fainting.
What Is the Two-Week Wait After Ovulation
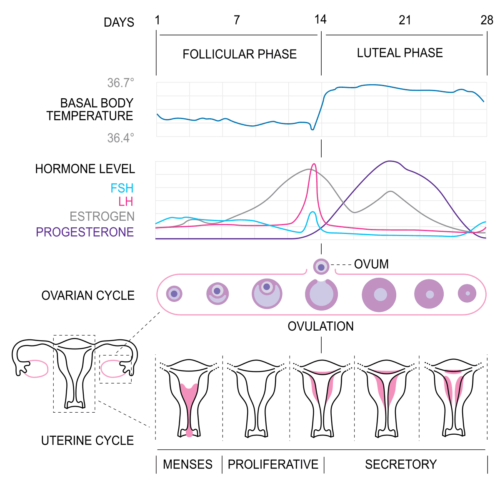
The two-week wait is the luteal phase, the window between ovulation and the start of the next period. After the egg is released, it can be fertilised for about 12 to 24 hours. Sperm can survive in fertile cervical mucus for up to five days, which is why sex in the days before ovulation can lead to conception. If fertilisation occurs, the embryo travels to the uterus and may implant several days later. If not, the hormone progesterone falls, the uterine lining sheds and a new cycle begins.
This phase often lasts 12 to 14 days for many people, but it can vary. Regular cycle tracking makes it easier to identify ovulation and gauge when to test. Apps, ovulation predictor kits, basal body temperature charts and cervical mucus observations can be used together to build a clearer picture of your timing.
The two-week wait can feel longer than it is. Understanding the usual sequence of events helps you avoid over-reading every change and helps you choose the best day to use a pregnancy test.
What Happens Day by Day After Ovulation
Fertilisation usually happens close to ovulation if viable sperm are present in the fallopian tube. Over the next few days, the fertilised egg divides into a cluster of cells while moving toward the uterus. Around day 5 after ovulation, the embryo reaches the blastocyst stage and begins to prepare for attachment to the uterine lining.
Implantation generally happens between day 6 and day 10 after ovulation. Once implantation begins, cells that will form the placenta start producing human chorionic gonadotropin, known as hCG. This hormone tells the ovary to keep making progesterone, which maintains the uterine lining. hCG rises over time and can be detected in urine a few days after implantation in many pregnancies.
Not everyone has the same timeline. Some embryos implant a little earlier or later, which affects when a test becomes positive. Light spotting can occur with implantation, though many people have no bleeding. Mild cramping or feeling warmer can occur, but these signs do not prove pregnancy on their own.
The Role of Hormones: Progesterone and hCG
Progesterone is the dominant hormone after ovulation. It thickens and stabilises the uterine lining and slightly raises basal body temperature. In the brain, progesterone can cause sleepiness and mood shifts. It can also lead to bloating, breast tenderness, constipation and mild cramps. These effects can be felt in both pregnant and non-pregnant cycles.
Once an embryo implants, the placenta begins to release hCG. This hormone supports ongoing progesterone production and helps the pregnancy continue. In early pregnancy, hCG usually increases over time. The rate of rise varies between people and between pregnancies. Urine tests detect hCG when it reaches a certain level. Blood tests can detect lower levels and can be repeated to check how levels are changing.
Hormone changes can be subtle or obvious. Having strong symptoms does not guarantee pregnancy. Having no symptoms does not rule it out. The most reliable way to confirm pregnancy is a properly timed test.
How Pregnancy Is Confirmed in Australia
At home, you can use a urine pregnancy test from the first day of a missed period or 14 days after ovulation. For those with irregular cycles, waiting at least 21 days after unprotected sex can also give a reliable result. Early testing can be negative even when pregnant, because hCG may still be too low to detect.
If you prefer a clinical check, a GP can order a blood test that measures beta hCG. This can detect very low amounts of the hormone. If needed, the test is repeated after about 48 hours to see if the level is rising as expected. If there is pain or bleeding, your GP may arrange a pelvic ultrasound once the pregnancy is far enough along to be seen on a scan, usually around six to seven weeks from your last period.
In Australia, early pregnancy assessment services exist in many hospitals for people with pain or bleeding in early pregnancy. Your GP or a health helpline such as Healthdirect can advise where to go. If you feel unwell or have severe symptoms, seek urgent care.
What Home Tests Involve and How to Use Them
Pregnancy tests measure hCG in urine. Sensitivity varies between brands. For the clearest result, test from the first day of a missed period and use first morning urine. Avoid drinking a large amount of water before testing. Read the result within the time window stated in the instructions, since lines that appear later may not be accurate. If a test is negative and your period does not arrive, repeat the test after 48 hours.
Ovulation predictor kits detect a surge in luteinising hormone, known as LH, that occurs before ovulation. Testing once or twice a day as you approach the middle of your cycle can help identify your most fertile window. Some people with conditions such as polycystic ovary syndrome have persistently raised LH, which can make results harder to interpret. Tracking basal body temperature and cervical mucus alongside ovulation testing can provide extra confidence in timing.
If you are unsure how to read a test, ask a pharmacist or GP. Choose tests from reputable suppliers that meet Australian standards and follow the instructions closely.
Managing Symptoms and Self-Care at Home
Good self-care helps many people feel more in control during the two-week wait. Aim for consistent sleep, regular meals and gentle movement. Consider a daily prenatal vitamin with 400 micrograms of folic acid at least one month before trying to conceive and continue it once you are pregnant. If you drink alcohol, consider avoiding it while trying to conceive. Limiting caffeine to about two small coffees a day is a practical approach for most people.
Mild cramps can respond to rest, heat and hydration. Paracetamol can be used for pain relief as directed. If you might be pregnant, ask a GP or pharmacist before taking anti-inflammatory medicines such as ibuprofen. Strong pain that does not settle needs medical review.
Worry can build during this time. Relaxation breathing, short walks, reading and short check-ins with a friend can help. If you feel persistently anxious or low, speak to your GP. Support is part of good fertility care and is appropriate at any stage.
When to See a GP, Fertility Nurse, or Specialist in Australia
Seek urgent care if you have severe one-sided pelvic pain, shoulder tip pain, heavy bleeding, fainting, fever or foul-smelling discharge. These symptoms can indicate problems such as ectopic pregnancy or infection and need prompt assessment. If you have light bleeding and mild cramps, speak to your GP for advice on monitoring and follow-up.
Book a GP visit if your period is more than a week late with repeated negative tests, if your cycles are very irregular or absent, or if you have ongoing pelvic pain. A GP can order blood tests, ultrasound and semen analysis for your partner if needed. If you are under 35 and have tried for 12 months without success, or 6 months if you are 35 or older, ask for a fertility workup and a referral if appropriate.
People with endometriosis, polycystic ovary syndrome or thyroid conditions may benefit from earlier assessment. In Australia, Medicare can cover many tests, and your GP can guide you to local services, including early pregnancy assessment units and fertility clinics when needed.
How Fertility Tracking and Tests Fit Into Your Plan
Fertility tracking helps you use your most fertile days well and reduces guesswork during the two-week wait. Observing cervical mucus that becomes clear and stretchy can indicate rising fertility. A positive ovulation test can signal the LH surge that precedes ovulation. Recording basal body temperature on waking shows a small rise after ovulation, which confirms that ovulation likely occurred. Used together, these methods make it easier to time sex in the days before ovulation and on the day it occurs.
During the two-week wait, avoid over-testing. Reserve pregnancy tests for the day your period is due or later. If a test is negative but your period has not arrived, retest after 48 hours. If results are inconsistent or you feel unwell, ask your GP for a blood test and advice.
Choose tools that are easy for you to use and interpret. Keep expectations balanced, since even with perfect timing it can take several cycles to conceive for many healthy couples.
What Pregnancy Tests and Blood Tests Show
Home urine tests report a positive result once hCG passes the test’s detection threshold. Different brands detect different minimum levels. A very faint line can be a true positive, but reading within the time window is important. Digital tests show words rather than lines, which some people find easier to interpret. Cost does not always equal sensitivity, so check the information on the box or ask a pharmacist.
GPs use serum beta hCG tests to confirm pregnancy. If needed, a repeat test after about 48 hours checks whether the level is rising as expected. A single number cannot predict the outcome of a pregnancy. Ultrasound is used later to confirm the location and assess growth. If there are symptoms such as severe pain or heavy bleeding, earlier review is important to check for ectopic pregnancy or other issues.
If results are unclear, your GP will guide next steps. This may include timing another blood test, arranging an ultrasound or advising watchful waiting.
Frequently Asked Questions About the Two-Week Wait After Ovulation Australia
Can stress stop implantation?
Usual life stress does not stop implantation. Very high stress can affect sleep, appetite and cycle regularity. Gentle routines that help you unwind are sensible during this time.
Do supplements like progesterone change test results?
Progesterone does not trigger a positive pregnancy test because tests detect hCG. Always use prescribed hormones exactly as directed and speak to your GP if you notice side effects.
Is exercise safe during the two-week wait?
Yes, moderate activity such as walking, swimming or yoga is fine if you feel well. Avoid new high-intensity training if it leaves you exhausted. Stop and seek advice if you have pain or bleeding.
Should I change my diet or caffeine intake?
A balanced diet and a prenatal vitamin with folic acid is recommended. Limiting caffeine to about two small coffees a day is a practical guide. If you drink alcohol, consider avoiding it while trying to conceive.
What if I have polycystic ovary syndrome and cannot detect an LH surge?
PCOS can make ovulation tests harder to interpret. Combine methods such as cervical mucus tracking and basal body temperature. Ask your GP about ultrasound or blood tests to confirm ovulation if needed.
Can early testing harm a pregnancy?
Testing early does not harm a pregnancy. The risk is a false negative or stress from uncertain lines. Waiting until your period is due reduces confusion and repeat testing.
Next Steps and Support During the Two-Week Wait in Australia
Staying informed helps you ride the ups and downs of the two-week wait with a steadier mind. Focus on what you can control. Keep a simple record of cycle dates, cervical mucus and any ovulation test results. Plan your test day for when your period is due. If your period does not arrive and tests remain negative, book a GP visit to discuss blood tests and next steps. If you have pain, heavy bleeding, dizziness or a high temperature, seek prompt medical care.
You do not need to make big changes to your life. Prioritise sleep, steady meals, movement and kind routines that calm your body and mind. A short chat with a partner, friend or counsellor can make this time feel more manageable. If you choose to use home ovulation or pregnancy tests, select trusted products and follow the instructions closely. A GP, pharmacist or fertility nurse can help you understand results and plan the next step that fits your goals.
References
https://www.healthdirect.gov.au/ovulation-and-fertility
https://www.healthdirect.gov.au/pregnancy-tests
https://www.healthdirect.gov.au/ectopic-pregnancy
https://www.healthdirect.gov.au/miscarriage
https://www.betterhealth.vic.gov.au/health/healthyliving/pregnancy-testing
https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/ectopic-pregnancy
https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/miscarriage
https://www.jeanhailes.org.au/health-a-z/fertility/understanding-fertility
https://www.jeanhailes.org.au/health-a-z/pregnancy/trying-for-a-baby
Evan Kurzyp
Evan is the founder of Fertility2Family and is passionate about fertility education & providing affordable products to help people in their fertility journey. Evan is a qualified Registered Nurse and has expertise in guiding & managing patients through their fertility journeys.